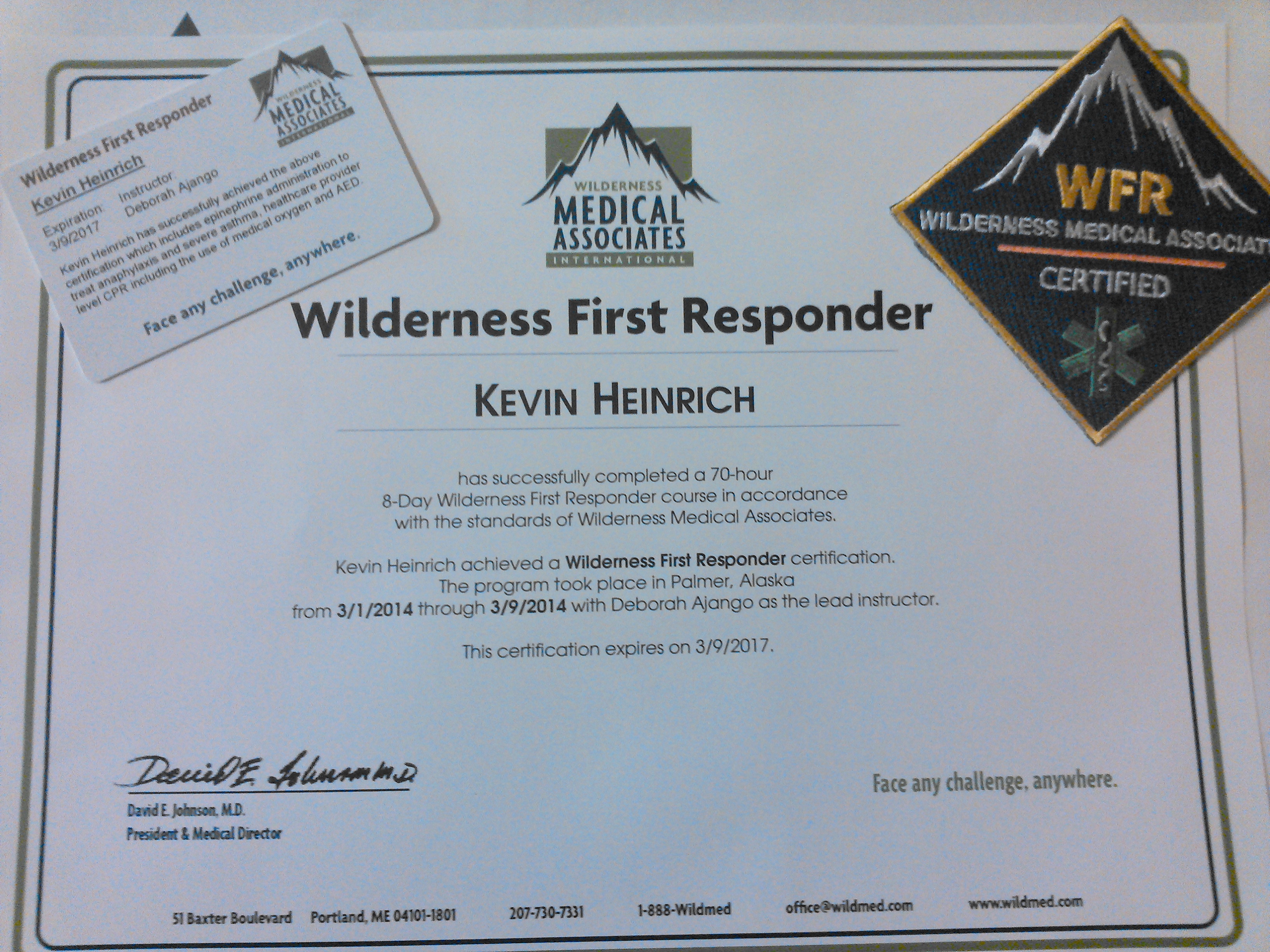
[I just received my Wilderness First Responder Certification from Wilderness Medical Associates. It’s a 70 hour 10 day course on backcountry medicine. I got the first 100% on the test in two years! Here’s the study guide I made and used. Good luck, stay safe!!!!]
Wilderness First Responder Study Guide
Circulatory:
Shock: Inadequate perfusion pressure in the circulatory system, resulting in inadequate tissue oxygenation.
Types of Shock:
Cardiogenic: “Pump Failure”; Caused by heart attack, chest trauma, or heart disease.
S/Sx: Chest pain/pressure with radiation, ↑Respiratory Rate, Variable Pulse
Tx: One adult aspirin, nitroglycerin as prescribed, PROP, gentle evacuation
Vascular: “Vessel Dilation”; Caused by anaphylaxis, heat stroke, toxins, or systemic infection.
S/Sx: ↑ Respiratory Rate, ↑Heart Rate, ↓Urine Output, NO shell-core
Tx: Treat cause. Horizontal position, hydration.
Volume: “Fluid Loss”; Caused by loss of blood or other body fluids
S/Sx: (Compensated) ↑Respiratory Rate, ↑Heart Rate, Shell Coring
(Decompensated)Very Rapid Heart+Respiratory Rate, ↓Level of Consciousness
Tx: Evacuate, Stop Volume Loss, Insulate, Hydrate, Elevate Legs
Nervous:
A change in mental status can be caused by trauma or by components of the STOPEATS acronym.
Traumatic Brain Injury (TBI):
S/Sx: Mechanism of injury + any loss of consciousness, amnesia, or, altered mental status.
Anticipated Problems: ↑Intracranial Pressure
Tx: Monitor for ↑ICP
Increased Intracranial Pressure (↑ICP):
S/Sx: Following a TBI; deterioration of mental status, persistent vomiting, or severe headache
Tx: Rapid Evacuation.
Sugars
Temperature
Oxygen
Pressure
Electricity (Seizures/Electrecution)
Altitude
Toxins
Salts
Respiratory:
Distress: Difficulty breathing, speaks in short sentences.
Failure: Only speaks 1-2 words at a time. A+Lethargic, V, or P on AVPU.
Arrest: No breathing. U on AVPU.
Parts of the system:
Upper Airway Problems: Blockages
Lower Airway Problems: Swelling due to irritant or histamine release. Spasm due to irritant (asthma).
Alveoli Problems: Introduction of fluids (breathing water, blood, vomit) or other irritants.
Chest Wall Trauma: Multiple broken ribs, puncture wound.
Respiratory Drive Problems (Brain): Hyperventilation (temporary), drive decrease-STOPEATS that cause disruption in brain homeostasis.
Asthma:
Treatment for someone in respiratory distress with history of asthma:
- Position best respiration
Reassurance, slow deep breathing
Oxygen, supplemental/seek best air
Positive pressure ventilations, Rescue Breathing if in Failure
- Meter Dose Inhaler as needed
Treatment for someone in respiratory failure with history of asthma:
1st 0.3mg Epinephrine
2nd 6-10 puffs of Meter Dose Inhaler
3rd 40-60mg Prednisone
4th Evacuate
Wounds:
The anticipated problem with any wound is infection; therefore, aggressive wound cleaning is necessary.
Wound Cleaning:
1st Clean/scrub around the wound with clean water.
2nd Wipe around the wound with 10% iodine solution.
3rd Tweeze out any large objects in the wound.
4th Irrigate the wound with clean water and increasing pressure, tweeze as necessary.
5th Once clean, allow 1% iodine solution to “pee” into the wound (no pressure).
6th Dress wound with sterile gauze damp with 1% iodine, wrap lightly.
Infection:
S/Sx: Increasing redness, pain, warmth, swelling after 24 hours (Localized). Fever, malaise, regional swelling, red streaks, vascular/volume shock (Systemic).
Tx: Incise/drain abscess, irrigate/dress, allow drainage, hot soak x4 per day, antibiotics, evacuate (Localized). Aggressive hydration, antibiotics, sugar, PROP, urgent evacuation (Systemic).
Musculoskeletal:
Stable vs. Unstable: A MS injury is unstable if: 1. It can’t be moved, used, or bear weight
2. It is deformed
3. There is impaired CSM’s
Treatment for a stable MS injury: Rest Ice Compression Elevation (RICE), splint/sling for comfort, NSAID’s for pain/swelling, monitor CSM’s.
Treatment for an unstable MS injury: Splint in position found unless ischemia+deformity, insulate, hydrate+food, monitor CSM’s.
Dislocations: Method of Injury must be torque/leverage not impact/crush, palpate to ensure there are no broken bones (exquisite pain). Only field reduce shoulders (baseball position), patella’s (push medially as you straighten leg), and digits (TIP).
Thermoregulation:
Hypothermia:
Normal Cold Response S/Sx: Shivering, A+O.
Mild Hypothermia S/Sx: Mental status change (still Awake), strong shivering, shell-core. Tx: Rewarming, food+fluids, insulate.
Severe Hypothermia S/Sx: V,P, or U on AVPU scale, shell-core, no shivering
Tx: Aggressive rewarming, urgent but gentle evacuation, food+fluids when possible
Heat Illnesses:
Heat Exhaustion S/sx: Subdued mental status, core-shell (red skin), sweating. Tx: Fluids, food, cooling.
Heat Stroke S/sx: Big mental status changes, vital signs for volume shock. A’: Volume shock, ↑ICP. Tx: Aggressive cooling, fluids and food, evacuation (urgent if not improving).
Frostbite/Frostnip:
Frostnip S/Sx: Patient can feel his extremity (poke with knife), pale/red. Tx: Rewarm, protect from trauma/refreezing.
Frostbite S/Sx: Hard, pale or blue skin, no feeling with knife poke. Tx: Rewarm if; immediate evac is impossible and extremity will not be used, and refreezing can be prevented. 600-800mg ibuprofen, pain control, bandage/splint, antibiotics, evacuate ASAP.
Anaphylaxis:
A histamine response to an ingested, injected, inhaled, or absorbed antigen.
S/Sx: Respiratory distress, hives, altered mental status, tight scratchy throat.
Tx: 1st 0.3mg epinephrine 2nd 25-50mg Benadryl 3rd 40-60mg prednisone 4th evacuate
Protocols:
Wilderness First Responders learn unique skills that can be performed under certain circumstances that urban professional rescuers cannot perform those skills are:
- The administration of prescription drugs for anaphylactic shock
- The administration of prescription drugs for severe asthma
- Reducing simple dislocations (shoulder, patella, digit)
- Assessing and clearing the spine
- Aggressive wound care and/or the removal of impaled objects
- Cessation of CPR after 30 minutes


4 Responses
Reviewed 4/13/2014
Hey thanks so much, this may be a few years old but still relevant.